FastTrack
A hyperlipidemia management system
[ Past project - Summary from 2007 ]
Despite evidence-based guidelines, cholesterol control in high-risk patients remains persistently sub-optimal. Barriers to effective control include an increasing burden of clinical data and limited time during clinic visits.
We conducted a randomized trial of an informatics-based system to lower LDL-cholesterol (LDL) in patients with coronary artery disease (CAD) or risk equivalents and LDL > 100 mg/dL. For each intervention patient, primary care physicians were alerted via a unique e-mail system linked to the electronic medical record that provided all the pertinent information on one screen: current LDL and trend of past results, medications and drug allergies, liver function results, co-morbidities, text of the last note, and decision support to predict LDL lowering by statin dose. This e-mail provided "one-click" on-screen order writing that allowed PCPs to do any one of the following:
- generate a new statin prescription and corresponding patient letter,
- generate a completed lab requisition form and letter to repeat a fasting lipid panel, or
- defer any action
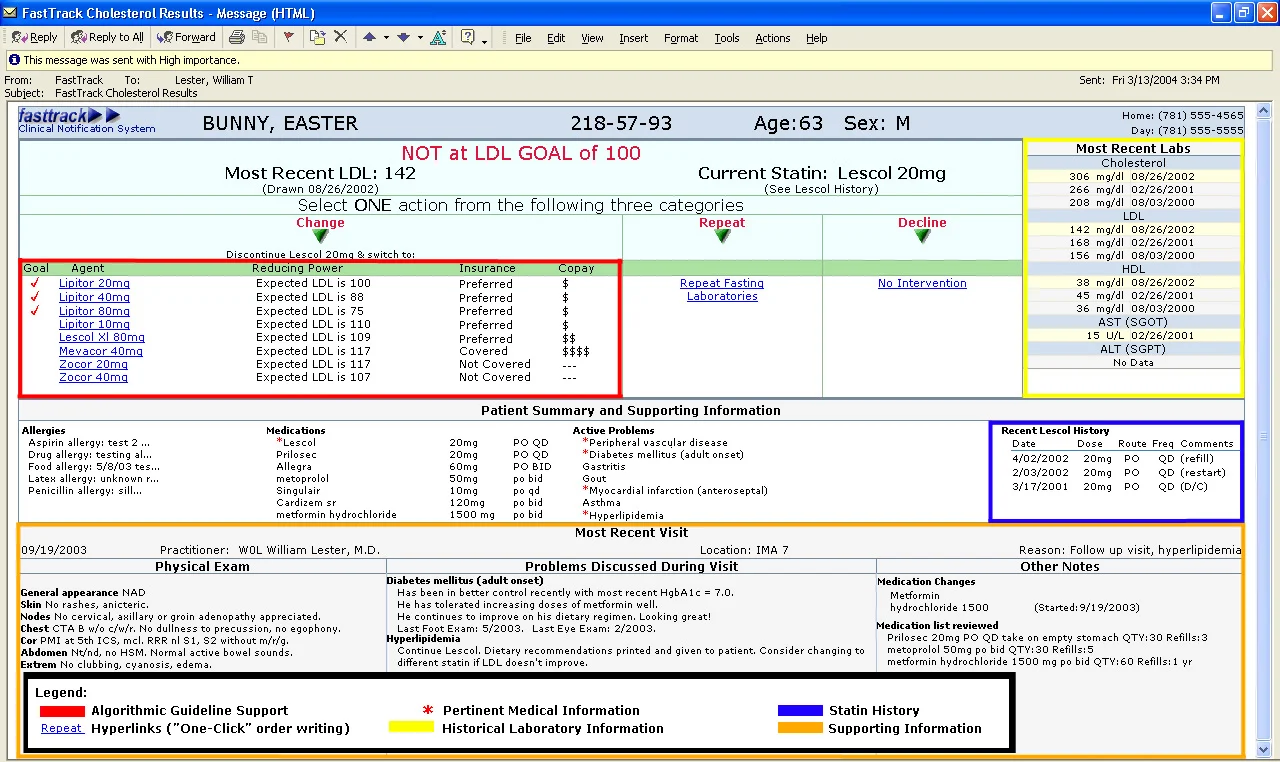
FastTrack screenshot: Click to enlarge
PCPs received no information regarding their control patients. Baseline LDLs were defined as the most recent test prior to the study's launch. Endpoint values were defined as the first LDL recorded 6 weeks after the intervention e-mail.
We enrolled 241 eligible patients with LDL > 100 mg/dL (64% women, 22% non-white race/ethnicity, mean age = 63.7 (14) years) cared for by 15 PCPs in one primary care practice. Baseline LDLs were similar in both groups (127 mg/dL vs. 126 mg/dL, p=0.79). At the 6-month time point, LDLs were available for 62 control (51%) and 64 intervention (53%) patients. This subset of patients had similar baseline LDLs (124 mg/dL intervention vs. 127 mg/dL controls, p=0.34). Endpoint LDL values were significantly lower in the intervention patients (106 mg/dL vs. 117 mg/dL, p=0.04). Although not statistically significant, a greater proportion of intervention patients reached LDL goal < 100 mg/dL (48% vs. 37%, p=0.19).
Our informatics-based system to reduce barriers to cholesterol care resulted in a statistically significant and clinically meaningful reduction in LDL levels.
